Inside Angle
From 3M Health Information Systems
An update on the Hospital Readmission Reduction program
At the end of September, CMS posted the latest round of data supporting the Hospital Readmission Reduction Program. This is the first year of compliance with the direction of the 21st Century Cures act to provide an adjustment for socioeconomic status (SES) in the measure. In our March blog on this topic we explained why the peer group adjustment is likely to be flawed—not because of the need for an adjustment—but because creating five peer groups based on SES is a highly imprecise way of making the adjustment.
Last week, Modern Healthcare returned to this issue2 following a study that they conducted in conjunction with Sullivan Cotter and Associates. The study and commentary fit much of what we expected in March. Peer groups have other shared characteristics, with specialty hospitals clustered in peer group 1 (highest SES) and large teaching hospitals in peer group 5 (lowest SES). As we demonstrated in our accompanying article, by having low volume hospitals in one peer group and high volume hospitals in another you begin by trying to adjust for SES, but end up adjusting for something else. In the example we gave, the something else was volume1.
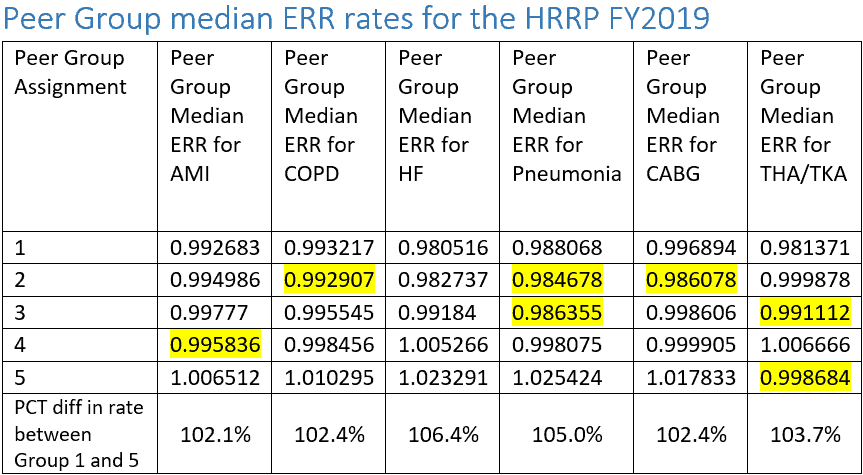
While the Modern Healthcare analysis focused upon changes in penalty status that could be tied to any number of additional reasons (of which one is the peer grouping), it helps to look at the specific drivers of the SES adjustment—the peer group median expected readmission rates (ERRs).
Source: FY 2019 IPPS Final Rule: Hospital Readmissions Reduction Program Supplemental Data File
The purpose of the SES adjustment is to provide relief for the obvious and oft found correlation between poverty and worse health outcomes resulting from structural community disadvantages outside of hospital control. We should therefore expect that as SES decreases (a larger percentage of poorer patients in the peer group) that the median ERR rate for readmission should increase. Since peer groups are labeled 1 through 5 with decreasing SES, this should result in monotonically increasing ERRs as the peer group number increases. In fact, in the ERRs reported by CMS (and displayed in the table above) we find that there are 7 groups across the 6 measures where the median ERR rates of lower SES groups are lower than those of the higher SES groups (i.e. they are set a tougher standard). Given that peer group 1 serves as a baseline this means that 7 out of 24 (29 percent) of hospitals are set standards above what should be expected.
Much of this is due to the very close proximity of ERR rates across the quintiles. In our work we saw more stratification in deciles but, most likely the CMS observed more problems with non-monotonic ERR rates (along with the argument of annual stability they put forth). In the bottom row we can observe the narrow span of ERR rates moving from peer groups 1 to 5 with only Heart Failure and Pneumonia having spans of 5 percent across the 5 peer groups. This bunching of ERRs means that the SES adjustment will remain lower than expected as echoed in the AAMC comments in the Modern Healthcare piece.
As stated previously, this is an important and necessary adjustment to get right. It not only delivers payment penalties but patient guidance in selecting hospitals. Peer groups are a poor way to achieve that objective and CMS should move rapidly to develop a person centric adjustment for SES. This would be particularly helpful if the SES measure incorporated elements amenable to intervention (e.g. housing status, transportation food access). In the mean time they should at least ensure that a median ERR can only be the greater of its peer group or the one immediately preceding it. This would at least stop some of the irrationality.
Richard Fuller, MS, is an economist with 3M Clinical and Economic Research.
References:
- Fuller RL, Hughes JS, Goldfield NI, Averill RF. Will Hospital Peer Grouping by Patient Socioeconomic Status Fix the Medicare Hospital Readmission Reduction Program or Create New Problems? Jt Comm J Qual patient Saf. 2018;44(4):177-185. doi:10.1016/j.jcjq.2017.10.002.
- Catellucci M. CMS’ readmissions program changes hit specialty hospitals. Modern Healthcare. http://www.modernhealthcare.com/article/20181005/NEWS/181009938. Published October 5, 2018.