Inside Angle
From 3M Health Information Systems
Migraines part 2: Rescue and prevention treatments
In my blog last month, Migraines Part 1: Seriously… It’s not just a headache, I provided some basic information about the seven basic types of migraines, causes and triggers and some interesting stats. In this month’s blog, I will share information on what every migraineur holds fast to: management and treatment.
Treatments
Migraine remains a poorly understood disease that is often undiagnosed and undertreated. Migraine medications don’t cure migraines, but it is possible to effectively manage migraines. As with any chronic medical condition, the goal is to manage the condition. Medications generally fall into two categories:
- Preventive – Medication taken daily to help reduce the number of migraine attacks. These types of meds are typically taken by patients experiencing more than two migraines per month.
- Abortive/Rescue – Rescue or abortive meds only treat symptoms of migraine after the attack begins. Also, many rescue medications currently available must be taken as soon as the attack occurs, or they may be less effective.
The class of drugs for treatment include: antipsychotic and antihistamines, anti-inflammatory, corticosteroids, anti-nausea, antiemetics, beta-blockers, calcium channel-blockers, ergotamine (DHE45), anticonvulsant, anti-seizure and triptans and more.
As stated in Part 1 of this two-part blog, Medicare and other carriers have specific guidelines regarding which treatments match the physician’s documented diagnoses (diagnosis list provided in Part 1).
Side Effects May Include…
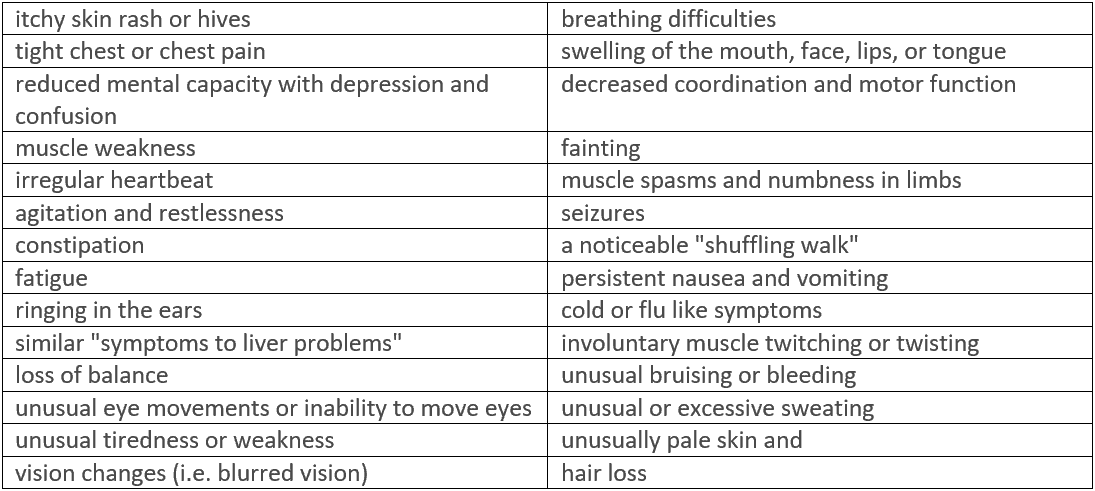
We’ve all seen drug commercials that rattle off the potential side effects of the drug. Migraine drugs are no joke and the side effects are not to be taken lightly. The goal is to find medications that work with the least amount of side effects. The following list, as noted by MigraineSavvy.com, seems to be the more general yet serious side effects listed for common rescue medications:
Yikes!! Reading this list may make you wonder why anyone would even take the meds!! However, I can tell you that most migraineurs will try ANYTHING at least once, if they think it may work. Many people have to go through trial and error with their meds and many rely on combinations of treatment options to provide effective migraine management.
WARNING! Medications could make migraines worse
Remember the saying, “too much of a good thing”? Migraineurs need to be extremely careful in the use of rescue medications or they may find themselves in an even worse situation. Too much migraine medication can result in what’s known as a “rebound migraine,” “medication-overuse headaches” or “chronic migraine,” causing a horrific cycle of migraine upon migraine. With each pill you take, you will start experiencing a shorter period of relief. Over time, you could develop a chronic migraine that will take weeks or months to wear off, once you cease medicating yourself. Medical professionals advise refraining from use of any type of migraine medication (even over the counter), more than twice a week.
New Hope with New Drugs
I’m not sure if you’ve heard, but there are new drugs available this year for migraineurs. I’ve even seen several different commercials advertising and promoting the new meds, What’s great about these new drugs is they aren’t rescue meds like triptans are (i.e. Imitrex) but preventive and they have been proven to work in patients who have had a lack of success with multiple previous preventive medications. Currently, three new CGRP preventive drugs are available.
So, what is CGRP? CRGP is the acronym for calcitonin-gene-related peptide. Migraine.com, American Migraine Foundation and other migraine websites describe CGRP as a protein that is released around the brain. When released, it causes intense inflammation in the covering of the brain and in turn, causes the migraine attack. These CGRP receptors are present in large numbers in the trigeminal system, the sensory nerves that supply the head and neck. It’s interesting to note that researchers have discovered CGRP is increased during a migraine attack and for people with chronic migraine, CGRP has been noted to be chronically elevated.
These CGRP blocker medications are the latest and (hopefully) greatest in migraine prevention. Here are the names of the drugs and their approval dates: (from Migraine.com)
- Aimovig™ (erenumab-aooe), approved by the FDA on May 17th
- Ajovy™ (fremanezumab-vfrm), approved on September 14th
- Emgality™ (galcanezumab-gnlm), approved on September 27th
How do they work?
In a Q & A session with Dr. David Dodick, Professor of Neurology and a headache specialist at the Mayo Clinic in Phoenix, Arizona, Chairman of the American Migraine Foundation and the President of the International Headache Society, he provided an easy way to understand how these new meds disrupt the CGRP process using a lock-and-key analogy—the CGRP peptide acting as the key and the receptor acting as the lock. While all three of these new products target the CGRP process, there are some differences between them:
- Aimovig blocks the lock, which allows less of the CGRP protein to bind to the receptors.
- Ajovy and Emgality attach to the key, distorting the CGRP protein so that less of it can connect to the receptors.
Not surprising, there is always the possibility of side effects with the new drugs that should be understood before beginning any of them. However, these new drugs are generally well tolerated with minimal/mild side effects. I encourage you to look up the side effects on the manufacturers’ websites to get the latest and most up-to-date information.
Will it work and what’s the cost?
No clinical trials were performed to compare these three new drugs, but the individual clinical trials showed similar results in terms of effectiveness, tolerability and safety. Each of the CGRP drugs have demonstrated the ability to reduce the number and/or severity of migraine days in adults with chronic or episodic migraine. As with all medications, some may experience relief and others may not.
The choice of starting a new medication should not be taken lightly and you should avail yourself of all the facts and have an informed discussion with your provider concerning options.
All three of these drugs cost about the same which works out to be close to $575 monthly. Coverage may vary of course by carrier and plan. There are assistance programs available (a couple months may even be free!). Again, this should all be part of discussions with your provider.
Personal experience and hope
As I stated in Part 1, I am a migraine survivor (there should be a diagnosis code for that!) I personally had my first injections of one of the new CGRP drugs in November. I will take them monthly. In addition, I was fortunate that my provider helped me get on an assistance program by providing the clinical documentation required. My current mind set is cautious optimism that I may be one of the lucky ones and see continued relief. In tandem with my other treatments (preventive and rescue), this may well be “my” golden ticket. Never give up!
Debra Jones is manager, coding analyst team for 3M Health Information Systems.
Sources:
Migraine.com
Headaches.org
MigraineSavvy.com
AmericanMigraineFoundation.org
MigraineReaseachFoundation.org
NationalHeadacheFoundation.org