Inside Angle
From 3M Health Information Systems
Migraines part 1: Seriously…It’s not just a headache
I am a migraineur| \mē-gre-ˈnər or mī-grā-ˈnər\. Merriam-Webster’s definition of a migraineur is an individual who experiences migraines. To me the word sounds like a cross between migraine and entrepreneur: a person who organizes and operates a business or businesses, taking on greater than normal financial risks in order to do so. So, my amended definition…. Migraineur: A person in the business of doing anything to manage/resolve their migraines.
Many people don’t realize that a migraine isn’t just a bad headache, or how totally incapacitating they can be. For many people, migraines are actually a chronic disease that impacts the overall quality of the person’s life. My intent for part one of my blog is to provide a very small peek into the world of migraines, and in part two I’ll talk about migraine treatment and some excitement over new preventive medications just released this year.
Let’s begin with some stats
- Migraine is a neurological disease with extremely incapacitating neurological symptoms affecting over 39 million people in the United States and one billion people world-wide.
- Migraine.com reports that migraines effect 87 percent of those who complain of some sort of headache.
- The World Health Organization has ranked migraine as the third most common medical disorder on the planet, out of over 300 different medical diseases.
- While typically most people experience attacks one to two times a month, more than four million people have chronic daily migraine, with at least 15 migraine days per month.
- Medication overuse is the most common reason why episodic migraines turn chronic.
- 90 percent of migraineurs are unable to work or function normally during their migraines.
Those are some pretty startling statistics! I’m not alone!
Physiology/Causes &Triggers
The National Headache Foundation states:
“While there are no definite answers to the causes of migraine, healthcare professionals are gaining an understanding of what happens when a migraine attack is in progress. Current theory suggests that migraines are triggered from within the brain itself. Once an attack begins, the pain and other symptoms of migraine arise from an inflammatory process resulting from an interaction between the trigeminal nerve and blood vessels in the coverings of the brain. Serotonin (or 5-hydroxytryptamine or 5-HT), a naturally occurring chemical in the brain, has been implicated in this inflammatory process.”
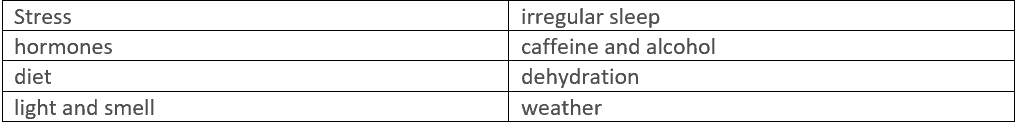
Triggers tend to have a theme for migraineurs and these signs can help identify patterns in your symptoms. Why is this important? It can help provide you with the information you need to manage future migraines. Everyone has different triggers, but there are a few common culprits that affect a large number of people living with migraine:
The American Migraine Foundation reveals that when it comes to sleep, nearly half of all migraine attacks occur between 4:00am and 9:00am. This puts people at a greater risk of developing sleep disorder on top of their migraines. And since sleep is a trigger you can easily fall into a cycle of which came first? Is it lack of sleep triggering the migraines or migraines preventing you from sleeping?
The one trigger that no one can control is the weather. Storms, excessive heat, humidity, and changes in barometric pressure are common weather-related triggers that can lead to a migraine attack. Almost half of migraineurs are sensitive to weather changes.
Frequency/Duration
Of course, everyone is different, but typically, migraine sufferers experience an average of two attacks per month, which can last anywhere from 4 to 72 hours. The National Headache Foundation notes that migraine attacks tend to occur in three phases: pre-headache, the headache itself, and post-headache. The pre-headache phase can last for several hours. The post-headache phase can last up to two days and can feature nausea, exhaustion and other mood changes. Who knew that migraines were so comprehensive and organized!
Migraine attacks may increase in frequency over time. Headache experts divide this process of transition into four distinct states:
- No migraine
- Low-frequency episodic migraine (less than 10 headache days per month)
- High-frequency episodic migraine (10-14 headache days per month)
- Chronic migraine (15 or more headache days per month, meaning that people with chronic migraine have a migraine or headache more often than not)
According to the International Headache Society’s ICHD-3 classification system, there are seven types of migraine:
- G43.0x – Migraine without Aura (formerly called Common Migraine
- G43.1x – Migraine with Aura (formerly called Classis or Complicated Migraine)
- G43.Bx – Migraine without Headache (can also be called acephalgic or optical migraine)
- G43.1x – Migraine with Brainstem Aura
- G43.4x – Hemiplegic Migraine
- G43.1x – Retinal Migraine
- G43.7x – Chronic Migraine
There are two migraine categories most people fall into:
- Migraine without Aura: This is the most frequent type of migraine. Symptoms include moderate to severe pulsating headache pain that occurs without warning and is usually felt on one side of the head. It comes along with nausea, confusion, blurred vision, mood changes, fatigue, and increased sensitivity to light, sound, or smells. Attacks typically last 4-72 hours, and they repeat a few times a year to a few times a week.
- Migraine with Aura: This type of migraine includes visual disturbances and other neurological symptoms that appear about 10 to 60 minutes before the actual headache and usually last no more than an hour. You may temporarily lose part or all of your vision. The aura may occur without headache pain, which can strike at any time. Less frequent aura symptoms include an abnormal sensation, numbness, or muscle weakness on one side of the body; a tingling sensation in the hands or face; trouble speaking; and confusion. Nausea, loss of appetite, and increased sensitivity to light, sound, or noise may proceed the headache.
Many patients may have more than one type of migraine or may not fall completely into one specific migraine category. There are also multiple co-morbid conditions that can occur. Medicare and other carriers are very specific regarding which treatments match the physician’s documented diagnoses (to be discussed in part two).
Personal Note: A Migraineurs outlook
I am a migraine survivor. I claim use of the word “survivor” over “sufferer” as a way to assert some measure of control over what has been one of the biggest challenges in my life and I’m sure in the lives of thousands of others.
Specifically, my diagnosis is G43.111, Migraine with aura, intractable with status migrainosus. Status migrainosus, or intractable migraine, is a persistent, debilitating migraine without aura that significantly affects a person’s ability to function. These migraines do not usually respond to abortive medications either. I’m also the lucky recipient of a second migraine diagnosis of Chronic Migraine G43.709, Chronic migraine (15 or more headache days per month, meaning that people with chronic migraine have a migraine or headache more often than not).
I’ve had migraines since I was 14 years old (I don’t want to do the math on how many decades ago that is). My migraines have put me through the ringer over the years with the challenges of dealing with and managing them. Many times, the frustration has been so strong I simply wanted to give up. However, if there’s one thing I’ve learned over the years, it’s that you have to keep trying and you can’t give up! You never know if the next treatment option just might be the golden ticket!
(Watch for my next blog, which will cover the latest in migraine rescue and prevention treatments)
Debra Jones is manager, coding analyst team for 3M Health Information Systems.