Inside Angle
From 3M Health Information Systems
Unspecified codes: Looking for patterns in denials
During the first 12 months of ICD-10, the Centers for Medicare and Medicaid Services (CMS) was lenient with ICD-10 coding specificity to allow providers to become accustomed to the new system and to promote a smooth transition. In this grace period, claims were not denied “based solely on the specificity of the ICD-10 diagnosis codes as long as the physician/practitioner used a valid code from the right code family.” This grace period expired on October 1, 2016.
According to the article “Improving Specificity in ICD-10 Diagnosis Coding,” in the April 2018 issue of Journal of AHIMA, nonspecific documentation and coding continue to be an issue, even though unspecified codes are necessary in some cases. According to ICD-10-CM Official Guidelines for Coding and Reporting FY 2018, “unspecified codes are to be used when the information in the medical record is insufficient to assign a more specific code.” In my opinion, this can be the case with testing, when lab work or cultures do not support the more specific code. In the case of laterality, however, it’s an issue of provider documentation. Examples of laterality issues can be seen in fracture, cyst, bursitis and neoplasm coding.
At present, neither CMS nor third-party payers are providing a list of unspecified codes that are unacceptable and likely to be denied, so HIM and billing professionals should review denials and watch for patterns to see which codes are triggering denials.
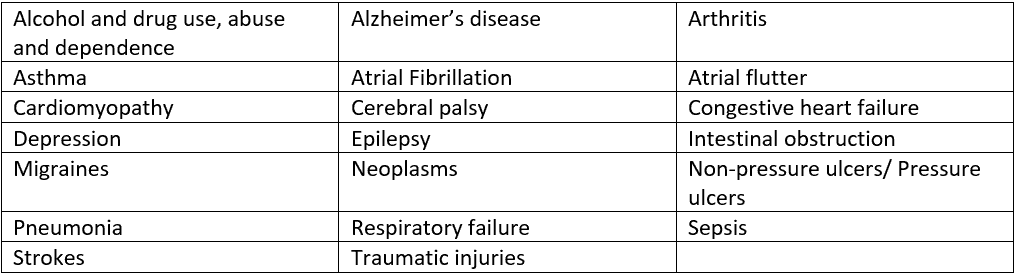
Facilities and/or providers should review the top codes causing denials to determine the underlying issue. If the issue is coder related, procedures may need to be developed or coder education undertaken on the importance of querying providers for more specific codes. The results of the audit can also be used to show providers the potential lost revenue that can result from unspecified documentation. According to the aforementioned article, there are 21 codes that are commonly reported as unspecified:
Coders have the knowledge and resources to support correct coding initiatives with official coding guidelines and/or facility coding procedures. Coders should continue to educate providers on the importance of clear and complete documentation for correct and specific coding. Continued good habits and detailed documentation practices will help lower denial rates. Ongoing collaboration between provider and coder are vital to the success of the facility.
Kimberly Lodge is a coding analyst for 3M Health Information Systems.