Inside Angle
From 3M Health Information Systems
ICD-10-PCS: Are we done playing catch-up?
AHA Coding Clinic’s Editorial Advisory Board (EAB) held its two-day winter session in February, and I participate on the EAB as part of 3M’s contract with CMS. As I was writing up my summary notes for the ICD-10-PCS topics on the agenda, I was happy to discover that not one of the topics we discussed resulted in change requests for the next PCS update—the first time in memory we had completed a session with no addenda for a future C&M meeting.
Coding Clinic has been publishing ICD-10 coding advice since 2012, well before ICD-10 implementation. During that time, especially in recent years, it seemed like every EAB session included at least one Q&A where the gist of the question was, “We know what we think the code should be, but we don’t see the [body part/ approach/ device/ qualifier] we want in the tables.” In these situations, the typical answer from the EAB is basically, “You’re right, the PCS code you want isn’t in the current version of the tables, so here’s what you should assign as a default.” Then this Q&A is published in Coding Clinic, so others with the same question will be assigning the same default code. Meanwhile, my job is to study the Q&A that brought the issue to our attention and send possible addenda proposals to CMS for consideration at the next available C&M agenda.
Below is a timeline that follows the life cycle of one such question, from coder question to proposed addenda to new codes:
2016, January, two-day EAB session—A question discussed during the session is for a lower artery bypass procedure from the right peroneal artery to a foot artery using autologous vein graft, and the peroneal artery body part value is not available in PCS table 041. After discussion, EAB consensus is to code according to PCS coding guideline B4.2, assign the closest proximal body part value which is the popliteal artery, and to publish the scenario. Here is the code included in the published answer:
041M09P Bypass Right Popliteal Artery to Foot Artery with Autologous Venous Tissue, Open Approach
During the meeting, I make note of a possible update to the PCS table 041 and follow up with CMS after the meeting, sending them mockups of proposed addenda options.
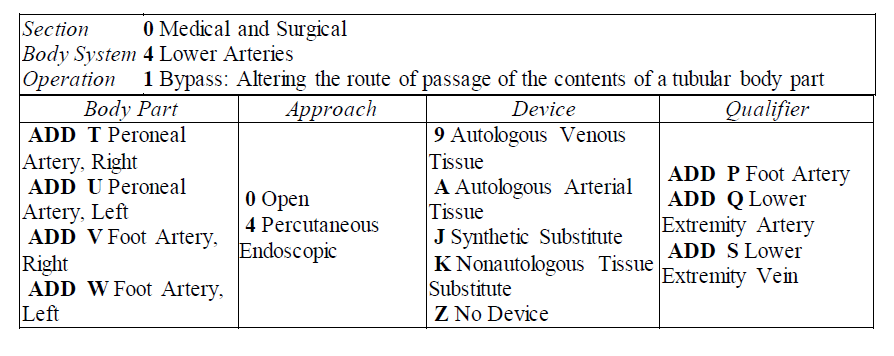
2016 September C&M agenda—In the addenda section of the meeting, there is a proposal to add the peroneal artery and foot artery body part values with their appropriate qualifiers to PCS table 041…”to capture detail for bypass procedures on the lower leg and foot arteries.” The specific values are shown in the proposal in hyperslice format, as 041[TUVW][04]^[PQS] (120 codes). The proposed change is also shown in the C&M agenda in a table mock-up format:
2017, 1st Quarter edition, AHA Coding Clinic p.32—The Q&A for coding advice on the peroneal artery to foot artery bypass is published. This explanation is included in the answer: “The body part is coded to the popliteal artery because although this is a peroneal artery bypass, there is not a body part value in table 041 for the peroneal artery. The popliteal artery is the closest proximal branch of the peroneal artery.” Versions of this explanation have typically been included in all Q&A’s in which the PCS tables are missing a needed value in the fourth through seventh characters.
2017, May, ICD-10-PCS update posted on the CMS website—The FY 2018 version of the ICD-10-PCS includes new codes for lower artery bypass, valid October 1, 2017. Here is the specific new code (one of the 120 codes proposed at the C&M meeting and which received public support in the comment period) for the procedure described at the beginning of this timeline:
041T09P Bypass Right Peroneal Artery to Foot Artery with Autologous Venous Tissue, Open Approach
2017, 4th Quarter edition, AHA Coding Clinic p.49—Code changes for the fiscal year are summarized in Coding Clinic every fourth quarter. For this change the summary reads, “In the Lower Arteries body system, root operation Bypass, body part values have been added for the peroneal arteries and foot arteries to capture detail for bypass procedures performed on the lower leg and foot arteries. This affects table 041, Lower Arteries, Bypass”and then the summary goes on to list the body part values and qualifiers that were added to PCS table 041 for the update.
There you have it—the life history for one change of many, many changes made during these first few annual update cycles to bring the PCS up to date. Like this one from 2016, some of the proposed changes were reported in the years since implementation, but many others were stored as backlog items during the code freeze.
The PCS table updates proposed as addenda items during these “catch-up” years since implementation can be broken down into three basic types:
1) Advances in surgical technique, such as the ability to bypass to more distant sites, or to use endovascular, catheter-based approaches instead of open surgical approaches
2) Omissions from the tables that were not found until the system was being used on a large-scale, and
3) Simplifications to improve data collection—for example, streamlining body part values in the PCS tables for structures where specifying right and left was a cumbersome distinction, as in the case of the frontal bone in the skull.
Back to my original “hurrah”—no new requests coming from the EAB. If we are getting caught up with the backlog of changes to PCS, does this mean we are done updating PCS? Nope. Not even. What I just described to you are only the things called “addenda items” in C&M parlance. They are the caboose of the C&M agenda. As I write this, the next C&M meeting is only a few days away, and “Addenda and Key Updates” is #17 of 17 topics. The other 16 are industry requests for specific procedure codes that uniquely capture technology/substances they have developed, or new surgical techniques.
Procedures will continue to evolve with advances in medical technology, and the innovators and pioneers will want specific codes to track how they are doing. So, although I for one will be happy to see the end of the addenda backlog, the code set will always be playing catch-up.
Rhonda Butler is a clinical research manager with 3M Health Information Systems.