Inside Angle
From 3M Health Information Systems
April OPPS update: More refinements to comprehensive APCs
Spring is here in the Rockies; the valleys are getting warm and the mountains are still snowcapped, making for a lovely view. With spring comes the April CMS outpatient prospective payment system (OPPS) update and my blog detailing some of the major changes. On a personal note, I retired from 3M HIS at the end of 2015 after almost 34 years, but I am back as a contractor and working to help customers stay up to date with OPPS.
So let’s talk about some of the April changes as they apply to comprehensive APCs (C-APCs).
Comprehensive APCs
It seems there is no end to the fine-tuning of comprehensive APCs (C-APCs). This April, the update not only includes some fine-tuning, but also a correction:
- Application of edits with C-APCs
- Items excluded from packaging
- Complexity adjustment when modifier 50 is coded
- Offset when no device is coded
- Correction to C-APC 5881
Edits and C-APCs
One might think that the C-APC is paid and everything else on the claim is packaged, with the exception of excluded items. That is to say, if some of the codes would normally be edited, but they wouldn’t be with C-APCs because they should be packaged. For example, if there were a service on a claim that would typically fail an NCCI edit, well it wouldn’t because it is packaged and the editing is then moot.
As the song says, “It ain’t necessarily so.” There are certain services that have specific status indicators indicating they are not allowed by CMS and shouldn’t be on a claim. If a HCPCS code with one of these status indicators is on the claim, the edit will process first and then normal processing will proceed. These status indicators are [definition from Appendix D1 OPPS files]:
- B [Codes that are not recognized by OPPS when submitted on an outpatient hospital Part B bill type (12x and 13x)]
- C [Inpatient Procedure]
- E [Not paid by Medicare when submitted on outpatient claims (any outpatient bill type)]
- M [Items and Services Not Billable to the MAC]
These status indicators elicit one of the following edits:
- 18 and 49 – related to inpatient services (LID – line item denial)
- 9 – Non-covered under any Medicare outpatient benefit, for reasons other than statutory exclusion (LID)
- 28 – Code not recognized by Medicare for outpatient claims; alternate code for same service may be available (LIR – line item rejection)
- 50 – Non-covered under any Medicare outpatient benefit, based on statutory exclusion (RTP – returned to provider)
- 62 – Code not recognized by OPPS; alternate code for same service may be available (RTP)
- 72 – Service not billable to the Medicare Administrative Contractor (RTP)
If the edit is a line item edit, that line will not pay, but the rest of the claim will process normally.
Edits 18 and 49 are line item edits related to status indicator C, and result in all services on the same date as the inpatient-only service being denied. If the claim also includes services on a different date, the rest of the claim will then process normally.
If the edit is a claim level edit, like the last three above, the entire claim will be impacted and returned for correction. The C-APC will also be impacted and receive no payment along with all other services on the claim.
Packaging exclusions
Let’s talk about those claims that don’t have any of these edits present, yet do have a C-APC. There are a number of items that are excluded from packaging. They fall into one of eight categories:
- Ambulance
- Brachytherapy (SI=U)
- Mammography
- Pass-through drugs, biologicals and devices (SI= G or H)
- Preventive care including influenza and pneumococcal vaccines (SI=L)
- Corneal tissue acquisition
- Certain CRNA services
- Hepatitis B vaccines (SI = F)
Pass-through drugs and biological services is the most dynamic group. Almost every quarter, APCs are introduced with a status indicator of G. This indicator is for drugs paid separately with pass-through status. Generally, they are paid using the same logic as other drugs paid separately with a status indicator of K. In this case, the difference is they do not package when billed with a C-APC.
With the April release, there are 10 new APCs. All of them have a status indicator of G. That means none of them would package if billed with a C-APC. Keep this in mind with each OPPS release when you see a new APC with a status indicator of G.
Complexity adjustments and C-APCs
C-APCs are assigned a payment rate that encompasses most or all of the services billed on the claim. In some cases, there are multiple codes that group to a C-APC and have a status indicator of J1, but only one will be paid. The OCE will determine which is to be paid based on a pre-set priority and the higher priority code pair will be selected and paid. In instances where there are two J1 codes, the one that is paid may receive a complexity adjustment and be paid at a higher rate. Whether there is a complexity adjustment or not is based on the code pair. CMS has defined a set of code pairs for which an adjustment is made. If the pair of codes on the claim is not on the CMS list, no adjustment is made.
Thirteen of the code pairs are actually two occurrences of the same code. If one of these codes appears two or more times, then a complexity adjustment will be made. These code pairs can be identified by the presence of the code on two separate lines, with one code being reported with units of two or more, or with one code reported with a modifier 50. The challenge, however, is that before the April release, modifier 50 would be ignored and not cause a complexity adjustment to be made, even though the modifier indicates the service was provided twice. This oversight has been corrected with the April 2016 release. (See the example below)
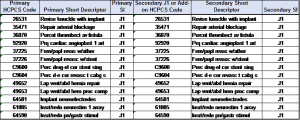
The thirteen codes on this list are listed in the table below (addendum J provides the whole list of code pairs):
When a C-APC is present, any associated device will be packaged. The exception is devices that have pass-through status, meaning have a status indicator of H.
In this case, the device is paid separately. Because payment for the C-APC includes dollars for the device, an offset amount will be applied to the C-APC payment to ensure there is no duplicate payment. Imagine CMS not wanting to pay for devices twice! I think we can relate to that.
Occasionally a C-APC will be billed with no device. In this situation, no offset will be applied. This seems obvious, but it was called out specifically in the April update.
Correction to C-APC 5881
This blog is getting long — are you still with me? I’ll be brief about the correction.
The April release corrects an error with C-APC 5881 (Ancillary Outpatient Services When Patient Dies). Prior to the release, some services that should have been paid separately and not packaged (see list above) were actually being packaged by mistake.
Example:
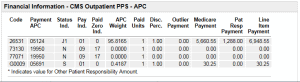
I wanted to share an example of some of the items we have discussed. Below are two tables. The first is a simple example with a C-APC, units = 1, no modifiers.
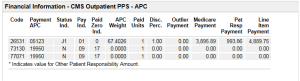
Notice the APC, weight and payment change for the J1 code, indicating that a complexity adjustment was applied because of the modifier 50 added to the code, illustrating the acceptance of the modifier.
Dave Fee is outpatient prospective payment consultant with 3M Health Information Systems.


