Inside Angle
From 3M Health Information Systems
“Ride it out at home?” Warning people at extreme risk of COVID-19, so they seek essential care
Julio Ayala died at home of COVID-19. I don’t know if he would have survived if he had gone to a hospital, but he might have. Nobody wants to be hospitalized. Many may fear hospitals, as that’s where the sick people go, but hospitals have geared up with procedures to prevent the spread of disease (including COVID-19) and in most cases, getting essential care may save a person’s life.
Riding out COVID-19 at home is a very risky proposition for people with a history of high illness burden. A person with severe chronic obstructive lung disease, plus complicated diabetes with heart failure is at extreme risk of bad outcomes compared to a person with uncomplicated diabetes and no other conditions.
When we consider how we might identify people most at risk, we must recognize that just flagging disease will give us an undifferentiated list of people with a wide range of risk. We can use administrative claims data to provide a much more nuanced understanding of which individuals fall into categories of “extreme high risk” and “high risk.”
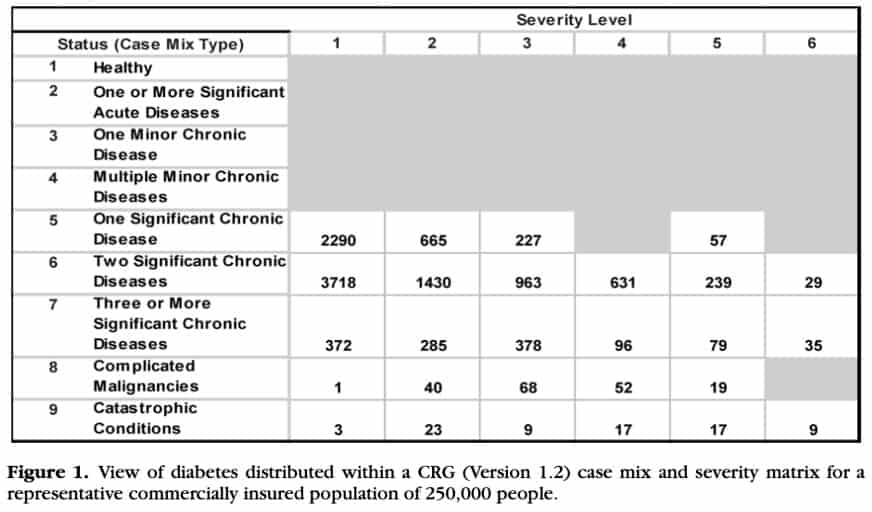
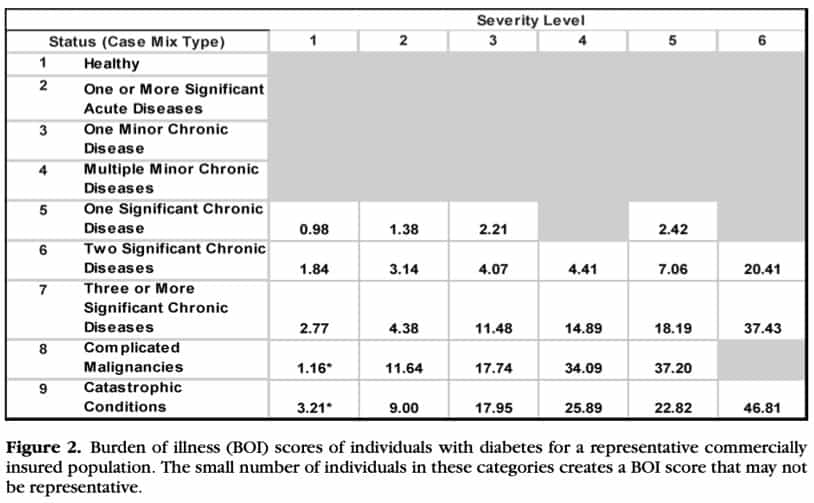
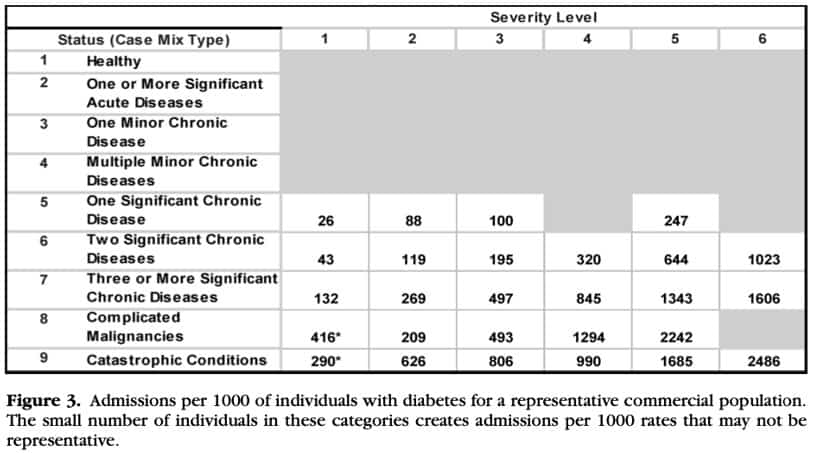
Below are three figures from an article by Bernstein describing how much more we can know about a population’s risk when we can segment that population by health status and severity. Figure 1 below breaks out a population of 250,000 to show how diabetes separates into distinct rows of health status and columns of severity. Each cell represents a group of people with diabetes with a different burden of illness and a different probability of poor prognosis. Figure 2 shows the total burden of illness for people in the cell compared to the average burden of illness for the entire population. Figure 3 shows the rate of hospitalization per 1,000 people per year for each cell.
When considering COVID-19 risk of poor prognosis, the nine status levels and severity levels from the Clinical Risk Groups (CRGs) can be used to identify significant comorbidity and high severity of illness individuals as shown in Figure 1. People with significant chronic comorbidities (CRG status 6 and 7) and people with severe underlying illness (CRG status 8 and 9) can be identified as high risk.
- Status 6 – Dominant or Moderate Chronic Disease in Multiple Organ Systems e.g., Diabetes, and COPD
- Status 7 – Dominant Chronic Disease in Three or More Organ Systems e.g., CHF, Diabetes, and COPD
- Status 8 – Malignancy, Under Active Treatment e.g., Lung Cancer
- Status 9 – Catastrophic Conditions e.g., Major Organ Transplant
This approach may be useful if you are thinking about sending an alert to those most at risk of poor prognosis, to say “Don’t try to ride this out at home” or “Maybe you don’t want to be in the front of the line for going back to work or having elective surgery” or “Please step to the front of the line when a vaccine becomes available” or if you have a supply of personal protective equipment to distribute it as they did in the Valencian community in Spain. [Read more on Valencian community use of COVID-19 tool].
L. Gordon Moore, MD, is Senior Medical Director, Clinical Strategy and Value-based Care for 3M Health Information Systems.
During a pandemic, healthcare information is gathered, studied, and published rapidly by scientists, epidemiologists and public health experts without the usual processes of review. Our understanding is rapidly evolving and what we understand today will change over time. Definitive studies will be published long after the fact. 3M Inside Angle bloggers share our thoughts and expertise based on currently available information.