Inside Angle
From 3M Health Information Systems
Medicare Advantage Star ratings and dual-eligible demographic rate adjustments – What’s next?
As a way to provide better care to beneficiaries and reduce federal health care expenditures, CMS rates each MA plan annually using the Star rating system. Star ratings are based on six different measurement systems spanning a broad array of metrics that capture clinical quality, plan service metrics and consumer survey data. Out of a five-star scale, it is critical for an MA plan’s success to earn Star ratings of 4 or 5 so it can gain maximum bid bonus payments and earn the right to market year round. Plans face many challenges when trying to increase their Star rating, but by focusing on the high-impact metrics they can create a common-sense improvement plan.
Areas which can have the greatest impact include: staying current on HEDIS changes, shifting focus from process metrics to outcomes and the sometimes overlooked pharmaceutical compliance metrics. Because they are updated annually, HEDIS metrics remain a moving target. These metrics are critical and account for nearly half of an MA plan’s Star ratings score. Health plans must remain vigilant in staying current with HEDIS changes so they are not taken by surprise during CMS reporting periods. Fortunately, MA plans that have also managed Medicaid plans are already tracking HEDIS metrics. MA plans can leverage the existing HEDIS infrastructure to support Star ratings as well.
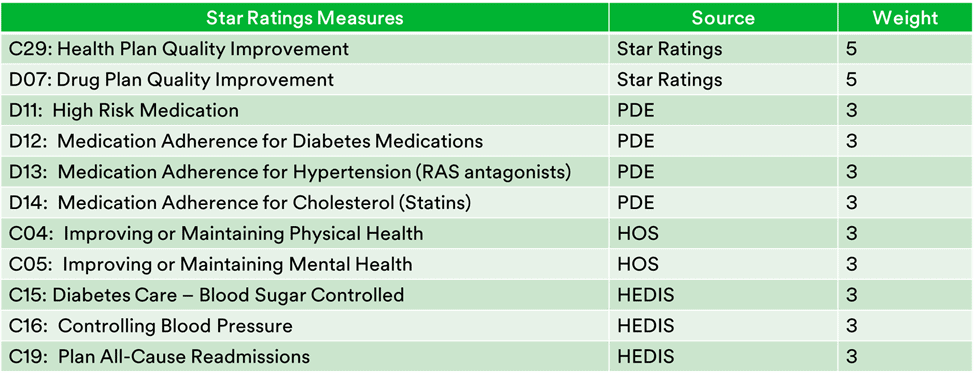
As alternative payment models place increased emphasis on quality, CMS now weighs Star outcome measures more heavily. This evolution has occurred quickly, and MA plans can now move the needle more by concentrating on the weightiest metrics to greater impact overall Star scoring. Here is a list of the top Stars metrics by weight:
A final area of MA plan focus for significant Stars improvement is pharmaceutical compliance. Four of the top eleven Stars measures relate to high-risk medication or medication adherence. Certain efforts, such as member educational programs aimed at sub-populations who don’t take their medicine as prescribed, can benefit the member’s health and the plan’s Star ratings.
You may be seeing stars by now, but this is not even an exhaustive list of the more than 50 Star metrics from Part C (Medicare Advantage) and Part D (pharmacy), but don’t fret! Plans can still use it to provide an effective road map toward improving Medicare Advantage Star ratings.
Dual-eligible Demographic Adjustments
CMS announced in the 2017 Advance Rate Notice and Draft Call Letter that it will adjust Medicare Advantage (MA) payment rates by adding six dual eligible related demographic adjustments and keeping the institutional adjustment. These seven demographic factors are:
- Community full benefit dual – aged
- Community full benefit dual – disabled
- Community partial benefit dual – aged
- Community partial benefit dual – disabled
- Community non-dual – aged
- Community non-dual –disabled
- Institutional
CMS’ intent with these changes was to more fairly compensate plans for higher risk, full benefit Medicare/Medicaid dual eligibles (FBMMEs). So, in that sense, this is a welcome change for the industry. As always, the actual impact of these changes will likely vary depending upon each plan’s enrollment demographic mix. I do not advise plans to rush out and try to enroll dual eligibles as these individuals are drawn from clinically complex, aged and disabled sub-populations that can be challenging to manage. The revenue related to dual eligibles is only one piece of the total picture. We do not yet know if the demographic premium adjustments will be sufficient to cover the higher expense of these members.
My advice to plans as plans prepare for 2017 is to try to take steps to assist MA members who are eligible but not enrolled to complete enrollment in the programs for which they are indeed eligible to 1) ensure that the plan is paid fairly by CMS and 2) support the member in fully accessing services to which they are eligible, including lower cost sharing for both Part C medical services and Part D prescription drug services.
Gretchen Mills is manager of market strategy for populations and payment solutions at 3M Health Information Systems.