Inside Angle
From 3M Health Information Systems
Hospital overcrowding: A complex but solvable problem
“…overcrowding is a hospital-wide problem that requires a hospital-wide response.”[1]
Overcrowding seems to be an ongoing problem for many hospitals in the U.S.[2] Overcrowding adds stress to physicians, nurses and other health professionals, can erode patient experience of care and have a negative impact on health outcomes.[3] What does it take to deliver care in a way that optimizes the trajectory of a person through a hospitalization, where that person receives the right care at the right time?
Achieving ideal “flow” through a system should result in improved outcomes and improved experience of receiving and delivering care. With optimal flow, work effort focuses on patient needs and is not wasted on poor communication and frustration with inefficient processes.
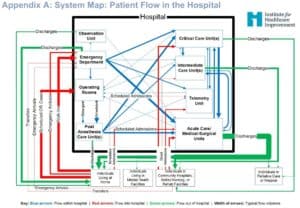
Appendix A below is a representation of patient flow in a hospital from an Institute of Healthcare Improvement white paper.[4] Given the number of points of demand and capacity it is not a surprise that efforts to improve parts of the system might actually degrade overall performance:[5]
An effort to reduce the number of emergency department boarders (individuals admitted to the hospital awaiting a bed) might move these boarders more expeditiously to a Medical Intensive Care Unit (MICU) only to create overcrowding in the MICU, causing the MICU to scramble to transfer patients to a step-down unit (SDU), which in turn causes the SDU to scramble to transfer patients to regular medical floors…and so on.
The IHI Hospital Flow whitepaper recommends matching capacity and demand using advanced analytics, integration of various quality improvement approaches, smoothing the load of elective surgeries and reducing demand while maintaining a focus on the overall system flow.
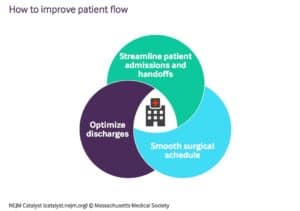
An article in the NEJM distills hospital flow efforts into three categories (see image below):
As noted in the opening quotation, hospital flow impacts the whole hospital and thus requires hospital leaders to make flow a high-level priority. If flow is managed by departments and units, these units will likely try to optimize their part of the system to the potential (and unintended) detriment of overall flow.
Achieving overall flow requires an ongoing stream of data to signal demand, matching that demand to the existing capacity, developing protocols to address surges in demand and redesigning work to reduce the impact of inefficient flow on patient outcomes. This work requires a combination of change management, process redesign, technology and advanced analytics.
L. Gordon Moore, MD, is Senior Medical Director, Clinical Strategy and Value-based Care for 3M Health Information Systems.
[1] https://www.commonwealthfund.org/publications/newsletter-article/focus-improving-patient-flow-and-out-hospitals-and-beyond
[2] https://www.beckershospitalreview.com/patient-flow/hallway-admissions-abound-at-overcrowded-montefiore-er-nurses-say.html
[3] https://journals.sagepub.com/doi/abs/10.1177/1062860608320628
[4] http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Hospital-wide-Patient-Flow.aspx
[5] https://hbr.org/2016/01/optimizing-each-part-of-a-firm-doesnt-optimize-the-whole-firm