Inside Angle
From 3M Health Information Systems
CareMore and Aspire Health bring their successful whole person care to Medicaid
Medicaid budgets are under extraordinary stress with increased enrollment, increased direct and indirect costs and declining state revenues. What can be done to mitigate these budgetary cliffs? Reducing unit prices usually leads to increases in the volume of services, negating the overall budgetary impact.
Value-based purchasing is an approach that could help. Medicaid agencies can move incentives from volume to value, providing clear programmatic signals that healthcare delivery can use to improve outcomes at the intersection of cost and quality.

What CareMore Health has done in Medicare can be done for Medicaid recipients, and CareMore and Aspire Health once again provide an example. They brought their comprehensive, relationship-based primary care model to Memphis, TN and Des Moines, IA and demonstrated millions of dollars saved at each location.
By moving away from fee-for-service incentives and focusing on people, CareMore Health can assess the needs of high needs/high cost patients and provide comprehensive care in collaboration with local non-medical resources.
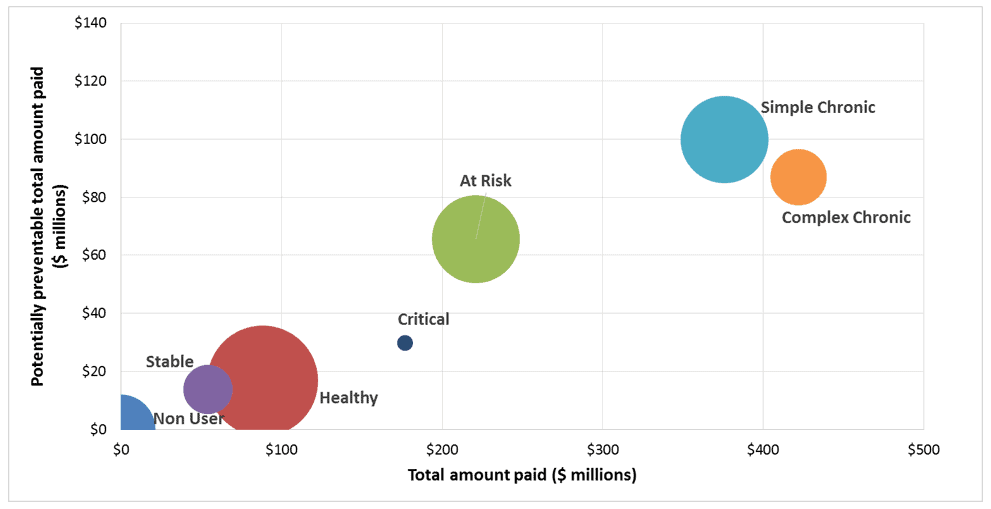
Figure 1 below demonstrates how a data-driven program can identify population segments with high needs/high costs, using aggregated Clinical Risk Groups in this instance to demonstrate population segments with simple and complex chronic conditions with high total cost and high potentially preventable costs (potentially preventable emergency room visits, inpatient admissions, etc).
Listen to Drs. Vibin Roy and Theresa Brown of CareMore Aspire Health describe their work with Medicaid recipients in Fort Worth, TX and the impact of that work on outcomes.
Figure 1: ~1million commercially insured all-sites-of-service de-identified claims data
L. Gordon Moore, MD, is Senior Medical Director, Clinical Strategy and Value-based Care for 3M Health Information Systems.
Watch Dr. Moore’s COVID-19 payer webinar archive: “Identifying individuals most at risk for poor outcomes.”