Inside Angle
From 3M Health Information Systems
Averages obscure important information: Who is at the greatest risk of mortality from COVID-19?
During a pandemic, healthcare information is gathered, studied, and published rapidly by scientists, epidemiologists and public health experts without the usual processes of review. Our understanding is rapidly evolving and what we understand today will change over time. Definitive studies will be published long after the fact. 3M Inside Angle bloggers share our thoughts and expertise based on currently available information.
Averages can obscure useful information. More nuanced information can be useful to care managers, for instance, or others looking to identify and work with high risk cohorts of people.
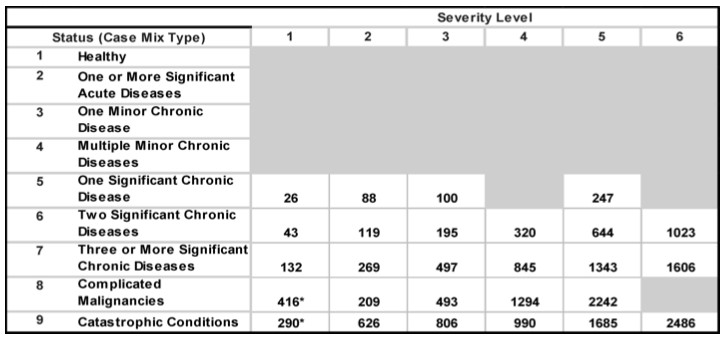
One study identified 631 hospitalizations per thousand people with diabetes per year. Looking further into this issue, another study found the probability of being hospitalized with diabetes varies dramatically with additional co-morbid conditions and severity. (See the study here.)
Table below demonstrates the rate of hospitalization per 1000 people with diabetes per year.
From this study, accessed 3/19/20
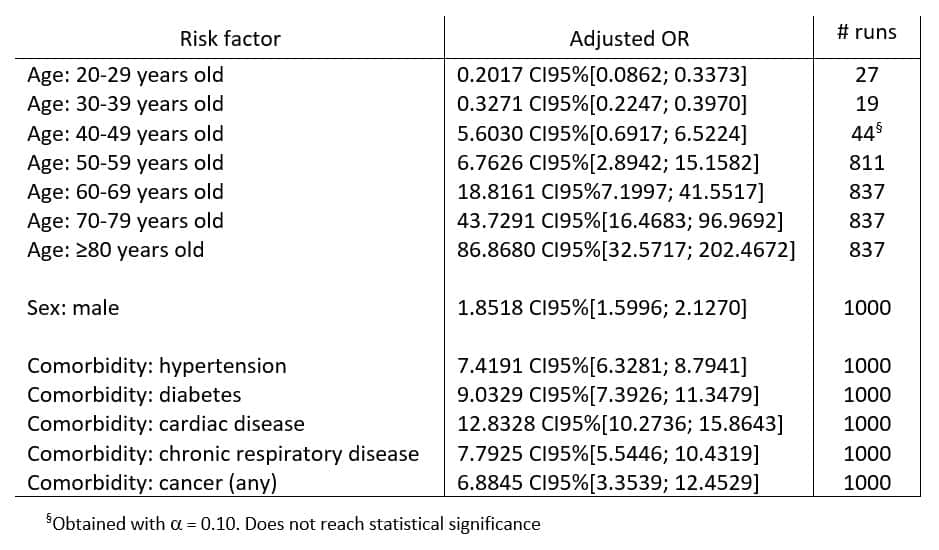
Average rates of mortality obscure the impact of COVID-19. Health plans and others can use longitudinal claims data to predict cohorts with high risk of death should they contract COVID-19 disease. We know that people with multiple conditions are at a greater risk for bad outcomes when compared to those with fewer or less severe conditions.
Mortality for people with confirmed COVID19 illness
Using mathematical modeling, one study based on China’s CDC data evaluated the odds of dying of COVID-19 infection for people with the disease. Compared to a person with no underlying conditions, someone who contracts COVID-19 and has diabetes is nine times more likely to die.
From this study, accessed 3/19/20
In-hospital mortality
The Lancet published a study of over 800 people admitted to two hospitals in Wuhan China, evaluating factors associated with increased mortality (among many other things).
Table 1 from the study shows the odds of death (compared to a person without comorbid conditions) for the people admitted to the hospitals. For example, a person with COPD admitted to the hospital with COVID-19, was found to have odds of mortality 5.40 percent greater than a person with no underlying condition.
|
Comorbid condition |
Univariable OR (95% CI) |
P value |
|
Chronic obstructive lung disease |
5·40 (0·96–30·40) |
0·056 |
|
Coronary heart disease |
21·40 (4·64–98·76) |
<0·0001 |
|
Diabetes |
2·85 (1·35–6·05) |
0·0062 |
|
Hypertension |
3·05 (1·57–5·92) |
0·0010 |
From this study, accessed 3/19/20.
Like all of you, we are working as quickly as possible to better understand the impact of this pandemic on populations. Using available (admittedly imperfect) data, we can place cohorts of people from claims data into risk strata to help those who, with scant time and limited resources, want to target outreach to the most vulnerable.
L. Gordon Moore, MD, is Senior Medical Director, Clinical Strategy and Value-based Care for 3M Health Information Systems.
Access a special webinar on COVID-19 featuring presenter Dr. Gordon Moore.