Inside Angle
From 3M Health Information Systems
Implementing CMS rule for 2019 – Evaluation and Management guidelines
One of the things that makes Tom Brady a great quarterback is his ability to think downfield. He’s not just thinking about the current play, but considering all the plays in advance. He is not focusing on one receiver but weighing all options. We are all waiting in a sort of limbo when it comes to the new CMS final rule proposal. How will we implement? Will the commercial payers follow suit as they usually do? I say, let’s look downfield and try to be as proactive as possible instead of reactive.
From the CMS final rule for 2019:
-For established patient office/outpatient visits, when relevant information is already contained in the medical record, practitioners may choose to focus their documentation on what has changed since the last visit, or on pertinent items that have not changed, and need not re-record the defined list of required elements if there is evidence that the practitioner reviewed the previous information and updated it as needed. Practitioners should still review prior data, update as necessary, and indicate in the medical record that they have done so;
-Additionally, we are clarifying that for E/M office/outpatient visits, for new and established patients for visits, practitioners need not re-enter in the medical record information on the patient’s chief complaint and history that has already been entered by ancillary staff or the beneficiary. The practitioner may simply indicate in the medical record that he or she reviewed and verified this information; and
-Removal of potentially duplicative requirements for notations in medical records that may have previously been included in the medical records by residents or other members of the medical team for E/M visits furnished by teaching physicians.
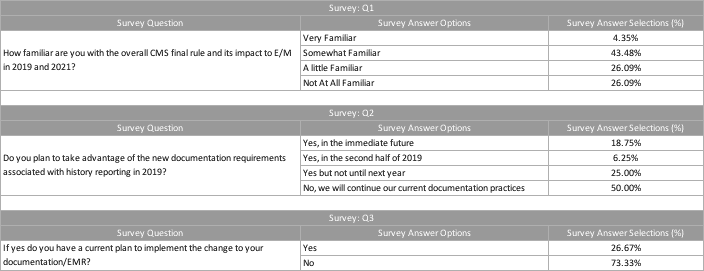
In a recent webinar provided to our 3M clients, we asked and receive responses to the following three questions:
Surprisingly (or not), the survey showed a large percentage of respondents were not even familiar with the new proposals. An easy and first step would be to get familiar! The changes will have a major impact on documentation for CY 2019 and documentation and revenue for CY 2021. In assessing the new guidelines, how do we operationalize and implement? I suggest making a list of stakeholders that will be impacted and then schedule meetings and discussions. Sometimes the first conversation is just a review of what is about to transpire. As we have seen from the industry, we are still coming to terms with the particulars regarding implementation of the proposal.
I like lists and to-do’s when working toward a goal. Here is how I would approach problem solving and implementing the current E/M guidelines:
- Start with the compliance department
- Engage physician trainers
- Review templates
- Schedule meetings with all stakeholders
- Reach out to your EMR vendor for any thoughts or best practices
Global thoughts and perspective:
- Have a template that scores the most points for private and Medicare payers.
- How can we accommodate CMS’s final proposal with the least amount of work? Could it be as easy as adding a sentence to the template?
Start the meetings and discussions now that 2019 is here and 2021 is not far off. Based on our coding analyst survey results, only 18 percent of respondents are going to take advantage of the new proposed rule. I have found it is far easier to be an early adopter of new proposals, rather than be reactive when I have waited to the bitter end. ICD-10 implementation taught me that lesson. In the back of my mind, I thought it would never come to fruition, and here we are! Proposed rules from CMS will happen as they have happened in the past.
Jean Jones is a coding analyst at 3M Health Information Systems.