Inside Angle
From 3M Health Information Systems
To lower readmission rates, focus on the intersection of cost and quality
A 55-year-old male is admitted to the hospital for an exacerbation of their chronic obstructive pulmonary disease (COPD). An 8-year-old child visits an emergency department with an asthma exacerbation. A 67-year-old woman ends up back in the hospital two weeks after a hip replacement. These are examples of potentially preventable events—events that might not have happened if appropriate interventions had been brought to bear in time.
Potentially preventable events highlight the intersection of cost and quality and are a focus for those interested in improving 
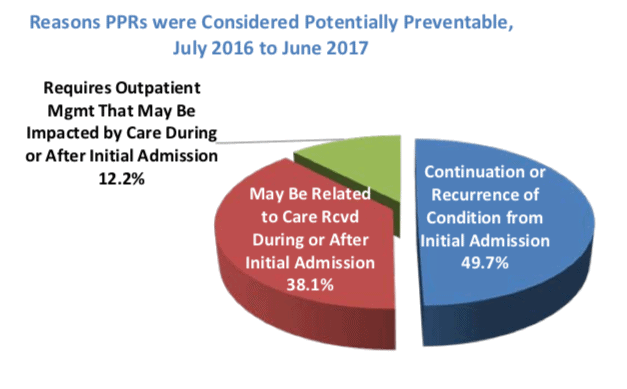
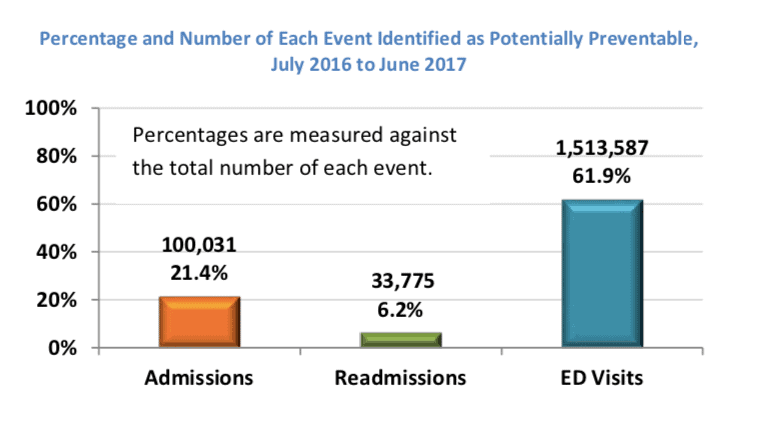
Below are some of the graphs in the report focusing on potentially preventable readmissions (PPRs). Florida Medicaid saw more than 33,000 readmissions in the year July 2016-June 2017.
BayCare Health System, headquartered in Tampa with 15 community-based hospitals, is an example of a Florida health system tackling readmissions. As its chief of quality, Teri Sholder initiated a number of programs aimed at reducing readmissions. She describes BayCare’s approach and their lessons learned in an Inside Angle podcast. What I found compelling in Ms. Sholder’s story is her ability to use data to drive decisions on which interventions to continue based on cost and impact.
Florida’s story is one example of a state’s intent to rationalize healthcare spending with a focus on the intersection of cost and quality, how that intent flows through the health insurance plans working in the state, and how healthcare delivery systems carry that intention through to changes in delivery that improve quality and costs.
L. Gordon Moore, MD, is Senior Medical Director, Clinical Strategy and Value-based Care for 3M Health Information Systems.