Inside Angle
From 3M Health Information Systems
VBP pilot programs underway in New York State
In New York State (NYS), as the final results for measurement Year 2 are solidifying, Value-based Payment (VBP) pilot programs are starting. The VBP pilots do not have an easy task in front of them with the various stakeholders (NY State, Payers, the PPSs) closely watching. Feedback from the VBP Pilots will not only be important in influencing the policy and analytic use cases, but more importantly, it will be used to set the tone for all other contracting entities. Having success in this project is vital to instill confidence in the statewide rollout. If the 3M experience is any indication, we know this program can have a positive impact on improving member experience(s) and quality, while lowering costs.
There are a number of considerations that are crucial in order to be successful and to achieve the ultimate goal of 80 to 90 percent of medical costs being under a value-based arrangement. Some of these considerations were previously blogged about on Inside Angle.
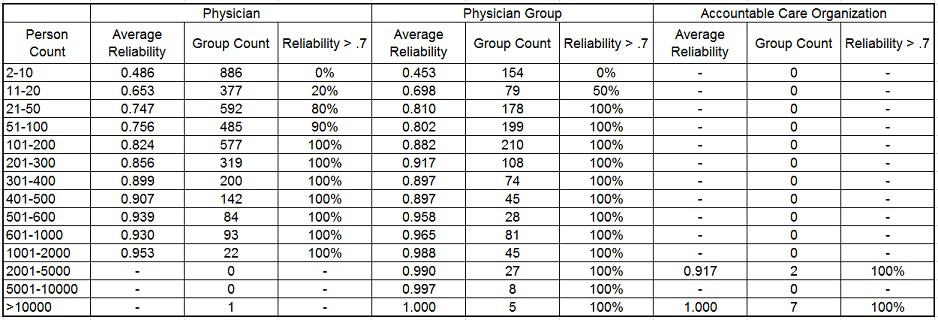
In the blog titled “Calculating reliability: Methodology adapted for estimating stability of cost data in New York,“ the reliability of provider groups with different attributed member sizes was discussed. This method was run on data sampled from a variety of payers and providers and under minimum eligibility month scenarios of 3, 6, 9 and 12 months respectively. Findings from this analysis consistently identified provider groups with 500 or more attributed members as being the reliability threshold for a stable sample size (where reliability > 90 percent). See the following table for an example.
Incorporating these results into the analysis of claims data, a provider group threshold of 500 members was set and sampling of health plan data was done. This was performed to determine what percentage of total medical cost would be captured within this threshold under value-based payment arrangements for these providers. On average, 72 to 75 percent of total medical costs were flowing through providers with 500 or more attributed members. This is only a marginal increase when compared to the expected value of 70 percent of total medical costs that would be included under provider groups with a minimum of 1,000 attributed members. However, the benefit is clear when considering the estimated rates are matched at less than half the expected sample size.
These results are not all that surprising to us. We have experienced similar patterns as we have helped our partners implement VBP programs. Some of our partners have had increased difficultly capturing an additional 5 to 10 percent without adopting new VBP policies or creating new programs. Through data analysis and strategy discussion, we have developed a number of “outside of the box” approaches to address this dilemma. One example of an approach was discussed by Shannon Garrison and Ryan Butterfield in their blog “Expanding VBP arrangements to meet requirements and medical ecosystems.” This blog discusses an option for gathering smaller provider groups into an entity that would have enough member attribution to create reliable measurement. This is an example of one approach that could be implemented to expand an existing VBP program to capture an additional 5 to 10 percent, engage smaller practices, and maintain reliability standards.
Although there is no official organization that brings these smaller practices together, our model for Medical Ecosystems allows for identification of practice patterns. This model is not only important to engage with providers that have less attributed members to help create reliable sample sizes, but also is an avenue to engage with specialists. Particularly within NYS, there are a number of VBP programs designed for specialists and episodic care. Not only are specialists significant contributors to patient care, they can also help move the needle on the 80 to 90 percent VBP objective.
One of 3M’s partners also used this method to target unattributed chronic users connected to specialists but not primary care providers (PCPs) and developed a strategy to engage those members. Since these members were already engaged in the virtual community, they were a natural fit to get connected to a PCP. This is an example of an additional strategy implemented to expand a VBP program within the same criteria and guidelines.
As VBP pilots ramp up, there will be more emphasis and interest in their implementation, design, and strategy. Succeeding in the short-term is equally important, if not more, than the long term strategy. Contracting with large provider groups (500 or more attributed members) not only ensures reliability, but also is a good starting point as they account for a large portion of medical cost. This approach may still fall short in terms of the total VBP objective, but strategies such as the model for Medical Ecosystems can be implemented to expand the program to achieve the goal. In the VBP pilots, it will be important to observe and leverage successes to determine the foundation for the long-term strategy, expansion and sustainability.
Matthew Ehlinger is a lead consultant with the Populations and Payment Solutions business of 3M Health Information Systems.