Inside Angle
From 3M Health Information Systems
HCCs for risk adjustment anyone?
The results of a recent study from the University of Michigan’s Institute for Healthcare Policy and Innovation on payment rewards and penalties for Michigan hospitals participating in the Medicare Comprehensive Joint Replacement (CJR) Program show that there are some improvements that could be made before the CJR program is rolled out more broadly.
Let’s take hip and knee replacements, for example. They are the most common inpatient surgery for Medicare beneficiaries, often requiring long rehab and recovery periods. There is also a wide variance in terms of cost and quality for these joint replacement surgeries among providers, and thus there is an opportunity to make a big impact by incentivizing hospitals to provide higher quality surgeries at lower costs.
Under the CJR program, Medicare sets a “bundled” payment amount for the full range of care provided to a hip or knee replacement patient, from the date of admission to the hospital through 90 days after discharge from the hospital. Rather than paying individual bills for parts of that care such as the operation, hospital stay and care after the hospitalization (physician therapy, for instance) the total cost of care is rolled up into one set amount. “Reconciliation payments” then reduce payments to hospitals if their spending is above a target (i.e. penalties) and increase payments if spending is below a target (i.e. incentives).
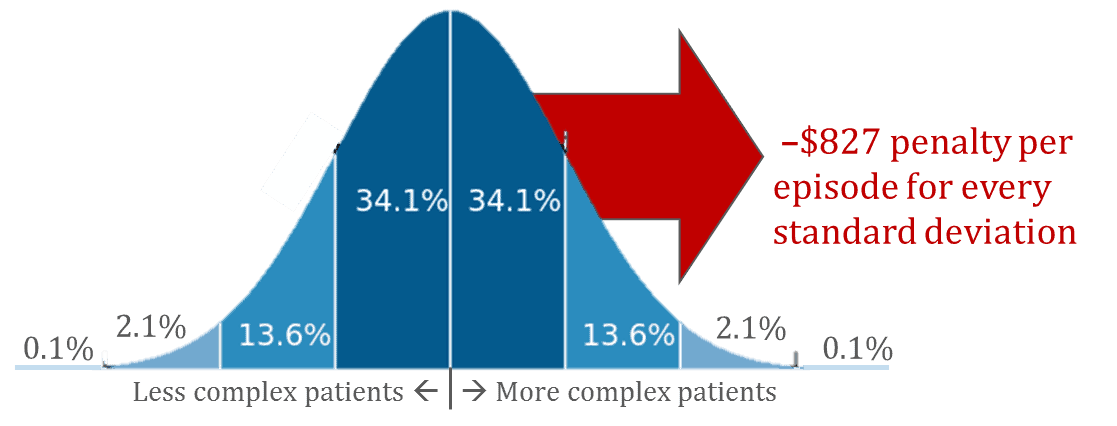
The University of Michigan researchers found that hospitals with sicker patient populations tend to be penalized more than hospitals with less medically complex patient populations under the CJR program guidelines. Granted, this was a simulation that modeled out the impacts of this program if it was applied to all hospitals in Michigan, but the results are pretty telling.
In this study the researchers found that every time a hospital’s patient population complexity increased one standard deviation from the mean, it ended up incurring a penalty of $827 per CJR episode.
When taking into account the varying levels of patient complexity that different hospitals handle by applying a risk adjustment model to these patients, some hospitals wound up keeping over $100,000 per year that they would have lost without the risk adjustment.
This amount may seem small when compared to many hospitals’ annual budgets, but if this bundled payment model moves beyond joint replacement episodes into other episodes of care such as cardiac surgeries or events, the numbers could become much larger.
Can you guess what risk-adjustment methodology the researchers used in their study?
Hierarchical Conditions Categories!
CMS uses HCCs as a risk adjustment and payment methodology in its Medicare Advantage programs, but did not use HCCs for the CJR program’s initial roll-out as it had not been fully validated for orthopedic bundles yet. This study could contribute to HCCs being heavily used for CJR.
Patient complexity is a key component that must be taken into account for any new value-based reimbursement and care model. HCCs have been proven effective under Medicare Advantage and with increased research and application will go a long way toward standardizing how programs take patient complexity into account to transform healthcare delivery and payment and ensure success for all providers.
Jeremy Zasowswki is marketing manager for 3M Health Information System’s Emerging Business Team.