Inside Angle
From 3M Health Information Systems
Expanding VBP arrangements to meet requirements and medical ecosystems
Following Medicare’s lead, New York State Medicaid has implemented requirements on health plans to rapidly increase the percentage of dollars being spent under value-based care arrangements. Not only will plans be expected to reach a goal of 80- to 90 percent of medical costs by 2020, but they will need to engage providers at three levels of participation. Most MCOs that 3M works with are well on their way in implementing strategies to engage in Value-Based Payment (VBP) and move toward shared risk.
Many plans have started signing contracts with large, well established Independent Practice Associations (IPAs) and provider systems, making headway toward value-based care targets. These large networks can help plans progress part of the way to the goal, but stop short of the 80 percent mark. In fact, to capture more than 60 percent of the medical expenditures, we have found that most plans will need a strategy to engage independent practices with a relatively small panel of members. This will also be a moving target as providers sign value-based care contracts, become more efficient and spend a smaller share of a payer’s dollars. Practices with panels numbering in the hundreds of members are harder to engage in value-based care arrangements because of the administrative burden and the need for critical mass to ensure quality and cost targets are measureable and significant. Small panel sizes can leave practices vulnerable to random outliers impacting outcomes. However, to be successful in meeting NY State’s targets, these smaller practices must be engaged.
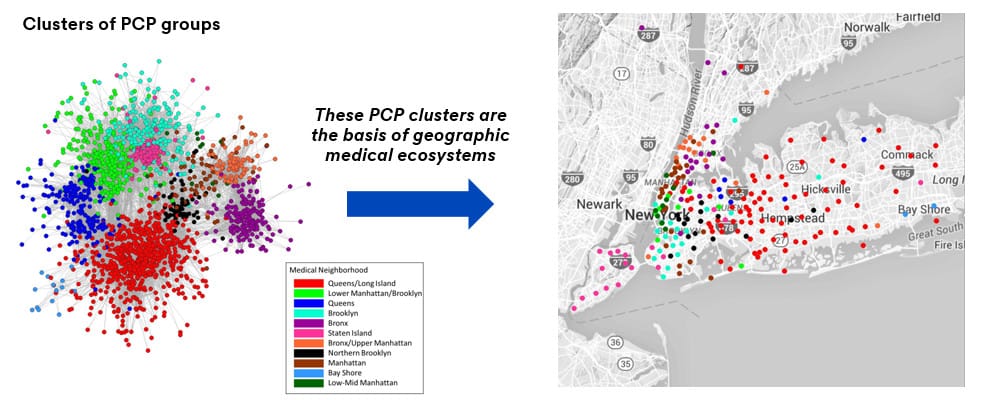
3M has researched how to use medical ecosystems to form a “virtual network” in an effort to engage small independent practices. This has been a topic of discussion for some time because these providers have been looking for an inlet to receive data that will help them improve quality and total cost of care measures. The first path we explored was a geographic based model. That allows for a grouping of practices, but there was a tremendous amount of variation in practice patterns among groups when they were aggregated on geography alone. These differences would make it hard to align performance incentives for the larger group. We then analyzed grouping on more than just geography by using the additional flexibility that a Social Network Analysis (SNA) approach allows. This method of analysis identifies which of the providers and specialists are treating the same populations while accounting for variation amongst the physicians.
SNA methodologies have long been utilized in the physical, medical and social sciences, and interest is growing in the social-behavioral fields. As part of quantifying 3M Medical Ecosystems, this proposed application to mapping the referral patterns of primary care physicians and specialists is new to the VBP landscape and unique to 3M HIS. SNA uses tools such as clustering metrics, graphical visualizations and regression techniques. Below is an example of how using the SNA to create 3M Medical Ecosystems can isolate separate clusters of provider groups and is reflective of affiliations that go beyond geography.
Value-based care arrangements can then be entered into with a virtual network created through SNA methodology. A larger structure would allow a path to distribute information as well as larger membership numbers for performance measurement. Since these providers are already working in a similar manner and in the same geographic area, they often have the same challenges and issues to overcome. Working with the data and with targets that are harder to make available without a larger grouping for a starting point, these providers can exist in a virtual network to obtain shared savings and higher quality care.
Ryan Butterfield, DrPH, MBA, senior researcher and statistician at 3M Health Information Systems.
Shannon Garrison consultant for populations and payment solutions at 3M Health Information Systems.