Inside Angle
From 3M Health Information Systems
Toward a health system reimbursement framework
There are many questions healthcare leaders across the Gulf are asking when exploring health system reimbursement options, including “What are the available innovative reimbursement models?”, “How to define successful reforms?” and “Will it work if it was working in other countries?”
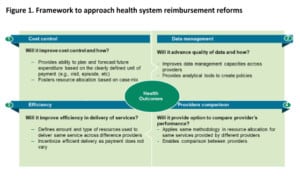
The answers to these questions are not straightforward. Clearly there is no single source of truth for successful reimbursement transformation. In an attempt to help health policy makers consider options in designing and defining a successful reimbursement reform journey, this article provides high level insights on how to utilize a five dimensional framework (four key and one cross cutting dimension). This reimbursement reform framework builds on the Institute for Healthcare Improvement Triple Aim framework, but it is focused on the reimbursement aspects of health system performance.
The proposed approach is straightforward. Each of the proposed five dimensions of the framework open questions and guide policy makers to look for the available evidence and international experience in order to find the appropriate answers.
Dimension 1: Cost control
Cost containment is one of the most critical questions in designing adequate healthcare reimbursement policy. Across the world, healthcare costs are rapidly increasing and exceeding the normal growth of the economy. This dimension of healthcare framework forces policy makers to answer critical questions such as:
- Will the newly proposed reimbursement model improve cost control and how?
- Can it help in planning future expenditures?
- How can it provide fairer resource allocations?
Addressing any of these questions will uncover different results depending on the reimbursement model selected. In a situation where policy makers consider pursuing prospective payment models such as DRGs (for inpatient services) or EAPGs (for ambulatory services), the primary responsibility for cost control is partially shifted from the payers towards the providers. This shift of risk is critical for the reimbursement reforms to achieve optimal cost control, as providers are left with the possibility of introducing innovative approaches in delivering required services at the most optimal cost.
Dimension 2: Data management
Another key dimension for any reimbursement reform is data management or answering questions such as:
- What type of data are required?
- Will the new reimbursement system improve data management and how?
- Can the newly acquired data be used for analysis and policy making?
Improving data management is another critical dimension of any health system reimbursement reforms. Reimbursement reforms must help both payers and providers get out of the “black box” and be able to clearly understand and estimate the cost of purchasing/delivering different types of services. This dimension should help decision makers understand if and how the new reimbursement model will support the health system to improve data management.
Dimension 3: Efficiency
Improving efficiency in delivering healthcare services should not be looked independently from cost containment, as these two are closely linked. On many occasions health providers may be able to improve efficiency, but they may not be able to control the cost. The most important questions to be answered here are:
- What is the optimal amount of resources that should be used in delivering a specific service across different providers?
- How does one decide the cost of efficient care delivery?
Shifting the financial risk is forcing providers to be much more practical in utilizing resources for delivering specific types of services. This contrasts with fee for services (FFS) arrangements where providers have no incentives to reduce any type of unnecessary care. If policymakers are looking to improve efficiency, they should consider exploring other reimbursement models besides FFS that would result in different types of incentives for providers (e.g., prospective patient classification systems such as DRG, EAPGs).
Dimension 4: Providers comparison
The fourth dimension is the capacity of the newly designed reimbursement reform system to provide a comparison between providers delivering the same type of services. This dimension helps policy makers to understand what resources different providers use to deliver the same type of services. Key questions for this dimension are:
- Are we comparing apples to apples when comparing different health providers?
- How does one select the most successful providers?
Providers comparison is important and if the results are published publicly it may incentivize the providers to improve their performance and outcomes.
Cross cutting dimension 5: Improve outcomes
Finally, the fifth cross cutting dimension is related to the improved health outcomes for the beneficiary population. In other words, will the newly designed reimbursement system help policy makers understand if population health is improving and/or learn if it helps lead to better health outcomes? For example, CMS uses seven groupings of outcome measures to calculate hospitals quality (mortality, safety of care, readmissions, patient experience, effectiveness of care, timeless of care, efficient use of medical imaging). Clearly, outcome measurement may be provided only if such data is available.
It is our hope that this framework will provide a small contribution in helping health policy makers deciding which way they should steer their health system reimbursement reforms.
Vladimir Lazarevik is lead 3M health economist across Middle East.